When Should You Reach Out to Your Navigator?
This article - written by Amplity's Sharon Gentry - was originally published in CONQEUR magazine
Navigators help patients and caregivers overcome healthcare barriers and provide them with timely access to quality medical and psychosocial care before a cancer diagnosis and through all phases of the cancer experience. The navigator can educate, remove barriers and facilitate access to care and resources, assess the patient’s needs, and provide emotional support.
Patient navigators function across the care continuum by providing a network of experts within the multidisciplinary care team, empowering the patient and caregivers in shared decision-making, and promoting best practices to ensure that the patient has access to evidence-based cancer treatment and the best quality of life possible.
Cancer Prevention & Risk Reduction
Education about cancer prevention and targeting risky behaviors for cancer are key tasks for navigators, as well as the promotion of health to the highest quality of life.
Healthy people with normal risk for cancer, and those with higher risk resulting from environmental and lifestyle factors, genetic predisposition, or precancerous lesions, can benefit from education on cancer prevention.
Navigators know the cultural and educational makeup of the community and can explain appropriate media and printed materials to the patient. They possess effective communication skills and can ask questions to help individuals identify personal goals and readiness to change behavior.
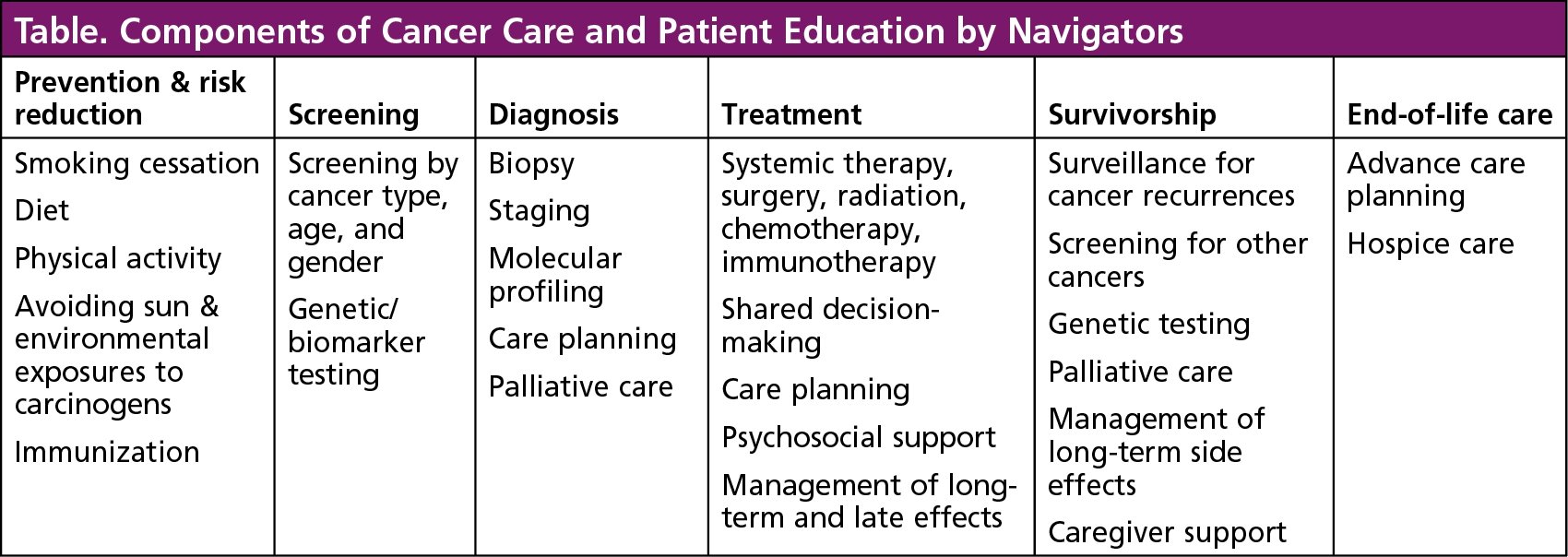
Many navigators are knowledgeable about smoking cessation programs, dietitians, physical therapists, and counselors who can address the myriad needs to improve a patient’s health. The Table outlines some of the key aspects of cancer education navigators provide to patients with cancer.
Misinformation
Reach out to a navigator if you need a speaker for cancer prevention and risk reduction. Or if you hear statements about cancer prevention or risks that you are unsure of, contact a navigator to get the right answer.
For example, patients often ask: Will cancer get worse if it’s exposed to air? The answer is No! Exposure to air will not make tumors grow faster, or cause the cancer to spread to other parts of the body. Another question asked is: Do antidepressants or deodorants cause breast cancer? Again, the answer is no. No study has found a link between chemicals found in antidepressants or deodorant and changes in breast tissue.
Cancer Screening
Navigators use national standards for age- and gender-specific guidelines related to the early signs of cancer, as well as community resources to improve patient access to cancer screening services.
Navigators are instrumental in improving cancer screening rates in low-income and racial or ethnic minority populations. The navigator is connected with the community, and with state or national programs that support cancer screening.
This outreach allows the navigator to conduct events with individuals, groups, and organizations at different settings, such as health fairs or cancer awareness events.
When you need to have a screening—for breast, cervical, skin, or prostate cancer, or genetic testing—the navigator can provide details of available services, ensure timely access to screening, and address any cost difficulties.
If you have questions or concerns related to transportation, insurance coverage, available times, cultural concerns, lack of understanding of the medical language, or just plain fear—call a navigator!
Navigators are there to not force you to go for screening, but rather to educate and empower you to make you own choice.
Diagnosis & Questions to Consider
Navigators are a bridge from a suspicious finding to an answer regarding a cancer diagnosis. Navigators reduce the time to diagnosis and increase the number of people who have diagnostic procedures.
Receiving a cancer diagnosis is an overwhelming event in a person’s life, so assessing the distress and providing psychosocial services is paramount at this time. A collaborative and trusting relationship between the navigator and the patient facilitates the removal of barriers to care, sharing education on the cancer and treatment process, and creates confidence so that patients can focus on making informed decisions and be active participants in their preferred care.
At this point, the navigator may ask you the following questions:
- What is your understanding of your current situation?
- How much do you want to know about your disease?
- What do you know, or have heard from others, about your cancer?
- Are there personal factors about yourself or your family that you wish to include in discussions about your cancer and its treatment?
- Do you want to have written information or an online source regarding your cancer?
- What is important to you?
- What are you hoping for in the future?
These questions set the stage to validate patients’ understanding regarding their diagnosis and treatment options, and open the communication between the multidisciplinary team, the referring physician, and other possible ancillary services, such as dietary, genetic counseling, rehabilitation services, and palliative care.
Treatment
Education is the key navigators will use with patients during treatment. Navigators are knowledgeable about treatment modalities, side-effects management, and multidisciplinary team members, as well as community resources to help patients through the treatment phase.
Many navigators are aware of a patient’s risk for side effects and late side effects when they screen, evaluate, and identify barriers to the patient’s care.
The navigator may ask what is your preferred method of learning—written, verbal, and/or pictorial? Navigators will often also ask you to repeat back in your own words what they have taught to ensure you understand the care plan. They will allow time for patients and their families or caregivers to ask questions, so don’t hesitate to ask any questions you have.
During this phase, navigators empower patients by educating them about anticipated events throughout the treatment trajectory and facilitate communication among providers, as well as between patients and providers, to have better coordination of care overall.
Patients’ needs evolve as their treatment progresses, so always be sure to get the navigator’s contact information, and feel free to reach out to your navigator with questions and concerns at any time.
Palliative Care
There is misunderstanding and lack of awareness about palliative care. People continue to use palliative and hospice care definitions interchangeably and regard both as end-of-life care; but this is not true. In reality, palliative care encompasses diagnosis, treatment, survivorship, and end-of-life care.
The Center to Advance Palliative Care defines this phase as specialized medical care for anyone living with a serious disease that focuses on providing relief from the symptoms and stress of the illness, with the goal to improve quality of life for the patient and for the family. Palliative care is based on the needs of the patient, is appropriate at any age and at any stage in an illness, and it can be provided along with curative treatment.
Palliative care doesn’t depend on prognosis or on life expectancy. For example, a newly diagnosed patient with breast cancer may have limited arm movement on the affected side of her cancer, because of an old injury that was never addressed. That patient will be referred to specialists, who will address this mobility issue so she could comfortably complete her breast cancer care, including surgery and radiation therapy that will require movement of that arm.
A patient with colon cancer often continues to have nausea after all treatment is completed, and the care team will help find a nausea medication that works, and involve a dietitian to create a diet plan to benefit the patient.
Palliative care can address pain, depression, shortness of breath, fatigue, constipation, nausea, loss of appetite, difficulty sleeping, anxiety, or any symptom that is interfering with one’s quality of life.
Navigators can help refer the patient to palliative care for symptom management and cancer rehabilitation, to supplement their care.
Survivorship
A cancer survivor is a person diagnosed with cancer from the time of diagnosis through the remainder of his or her life, but the survivorship phase is considered as the period after the completion of active treatment, whether surgery, chemotherapy, radiation therapy, or another type of therapy.
Navigators recognize that patients may feel a sense of abandonment by the oncology team as they transition to the survivorship phase and they don’t have frequent and consistent visits to the care facility anymore.
This is a phase in which patients are considered cancer-free, but they can experience late- or long-term side effects of treatment, such as fatigue, sleep problems, pain, peripheral neuropathy, difficulty concentrating, poor appetite, and decreased physical functioning.
Therefore, navigators have a role in education, assessment, and referral to resources to improve the survivor’s function and quality of life. They can connect survivors to rehabilitation services, dietitians, support groups, exercise classes, psychotherapists, and others to address the needs of the patient who is transitioning to a post-treatment world.
Hospice Care & End of Life
End of life is the phase when cancer treatment is no longer effective, and the cancer continues to progress. Navigators play an integral role in the transition of care to hospice care for patients who have a life expectancy of 6 months or less, and who are no longer receiving cancer-specific treatment, because their disease is deemed incurable.
Navigators will continue to evaluate for barriers, such as challenges within the healthcare system, financial concerns, and education needs. They will support the patient and the family as they plan for end-of-life care, and make sure that the patient’s voice is heard about his or her goals for quality of life and a good death.
Your navigator does not go away, but may step back, if hospice becomes the primary care service. The patient and the family need to reach out to hospice for primary needs.
Oncology navigators touch patients in any phase of their care and can provide an integrated, patient-focused approach to coordinate a personalized plan of care. The navigators are a knowledgeable source for resources and are familiar with the nuances of the healthcare system. They are an effective aspect of the patient-focused management throughout the continuum of care.